Key Takeaways: Your Recovery Roadmap
- Integrated Care is Best: Treating ptsd and alcohol abuse simultaneously yields better long-term results than treating them separately.
- Start Where You Are: You do not need to be completely abstinent from alcohol to begin effective trauma therapy.
- Proven Therapies Exist: Evidence-based methods like Cognitive Processing Therapy (CPT) and Prolonged Exposure (PE) are safe and effective.
- Flexible Options: Virtual and evening programs allow you to balance treatment with work and family life.
When PTSD and Alcohol Abuse Collide
Why PTSD and Alcohol Often Co-Occur
If you have ever wondered why ptsd and alcohol abuse are so often linked, you are not alone. Many people living with trauma find themselves reaching for alcohol as a way to quiet painful memories, numb anxiety, or simply get through the day. This coping style is sometimes called the “self-medication hypothesis.” It means that alcohol might temporarily dull the distress that comes with ptsd and alcohol abuse, but it often leads to bigger challenges over time.2
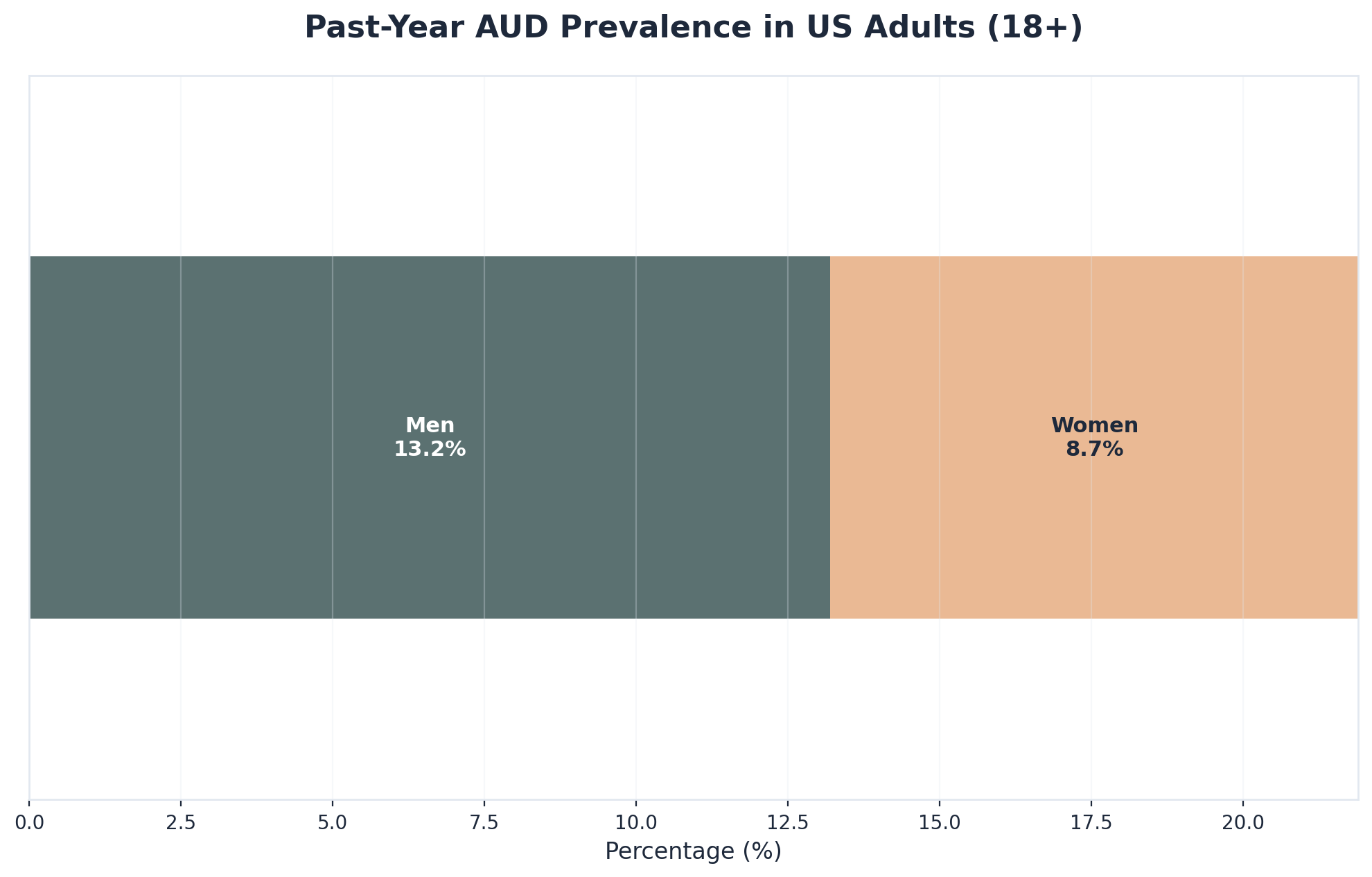
Research shows that between 30 to 60 percent of people with PTSD also develop a substance use disorder, with alcohol being one of the most common.1, 5 That is a huge number—and it is not because of weakness or lack of willpower. Trauma can change how your brain responds to stress, making it harder to feel safe or relaxed without outside help.
“Alcohol might seem like a quick fix, but it can actually make PTSD symptoms like nightmares, anger, or feeling on edge even worse.”
It is also important to recognize that ptsd and alcohol abuse often reinforce each other. While alcohol may numb pain in the short term, it can make healing from trauma even more difficult in the long run. The good news? You are not stuck in this cycle forever. Integrated treatment approaches are safe and truly effective for both conditions, and there is hope for recovery.1, 5 Next, we will talk about spotting the signs of this connection in your daily life, so you can take steps toward healing.
Recognizing the Signs in Your Life
Here is a simple assessment checklist you can use to spot the signs of ptsd and alcohol abuse showing up in your life. Ask yourself the following questions:

- Do you find yourself drinking more when memories or reminders of trauma surface?
- Are you using alcohol to help you fall asleep or calm your nerves?
- Have friends or family expressed worry about your drinking or mood swings?
- Do you feel irritable, on edge, or numb—especially after drinking?
- Are you having trouble remembering parts of your day or blacking out after drinking?
- Do you notice that your drinking is making your anxiety, nightmares, or sadness worse?
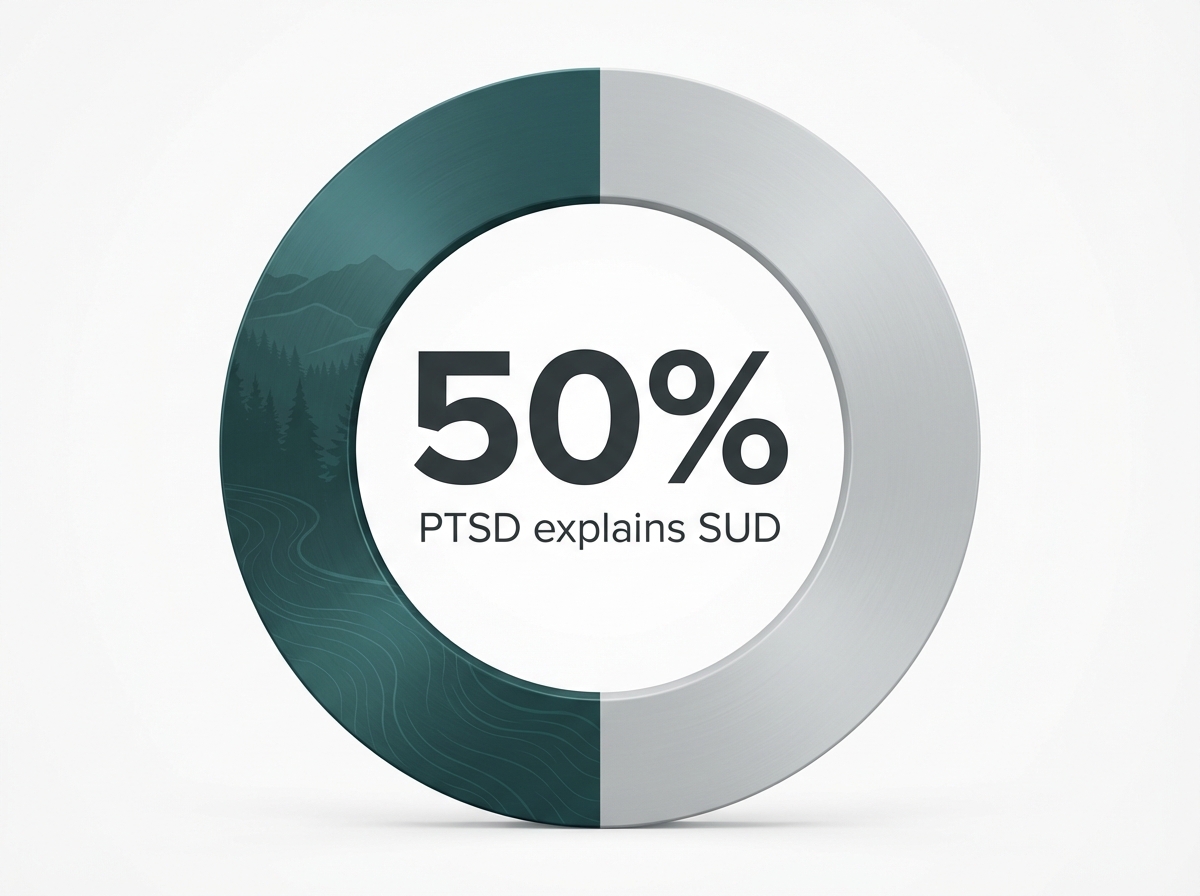
If you checked off several of these, you are not alone. Many people with ptsd and alcohol abuse experience patterns like these, and it is not a sign of failure. It is a sign that your mind and body are trying to cope, even if those coping skills are not giving you the relief you truly deserve. Studies show that more than half the improvement in substance use during recovery happens when trauma symptoms are addressed directly.2
Recognizing these patterns is brave. Every bit of self-awareness counts—each small insight can help you move toward healing. If these signs feel familiar, reaching out for support is a strong, hopeful choice. Next, we will explore why healing both trauma and alcohol use at the same time is so effective.
The Science Behind Integrated Treatment
Why Treating Both Conditions Together Works
Let’s start with a quick decision tool: If you are unsure whether to seek help for just trauma, just drinking, or both together, consider this—have you noticed that working on one makes the other flare up? If so, integrated treatment is likely the best fit for you.
Treating ptsd and alcohol abuse together means your care team targets both conditions at the same time, not one after the other. This approach is ideal for those who feel stuck in a loop—using alcohol to quiet trauma, but then finding that drinking makes memories and anxiety worse. Research shows that more than half of the progress people make in cutting down on alcohol actually comes from healing the trauma underneath.2 When both issues are addressed, you are more likely to see lasting change.
Some people worry that talking about trauma might set back their recovery from alcohol use. But the science tells a different story. Studies confirm that starting trauma therapy while still working to reduce drinking is not only safe, but leads to better results than treating one problem at a time.5 Patients do not need to be abstinent before starting trauma work—a major shift from older ideas about recovery.8
Consider this route if you have tried working on drinking alone and still feel haunted by past events, or if trauma-focused therapy has not helped because alcohol keeps pulling you off track. Integrated treatment respects your whole story and makes healing more possible. Next, let’s look at the specific therapies that help people recover from trauma while finding freedom from alcohol.
Evidence-Based Therapies That Heal Trauma
Let’s start with a practical tool: a therapy finder comparison. Ask yourself: Do you want to talk through painful memories in detail, or do you prefer to focus on changing how you think about your trauma? The table below breaks down the most effective options.
| Therapy Type | How It Works | Best For… |
|---|---|---|
| Prolonged Exposure (PE) | Gently guides you to process traumatic memories at your own pace to reduce fear. | People who want to stop avoiding triggers and reclaim their daily life. |
| Cognitive Processing Therapy (CPT) | Focuses on identifying and shifting unhelpful beliefs connected to trauma. | Those struggling with guilt, shame, or self-blame regarding the trauma. |
| Trauma-Focused CBT | Combines skills for managing distress with new ways of thinking about experiences. | Individuals who need practical coping skills alongside trauma processing. |
Research shows that 51% more people treated with CPT lose their PTSD diagnosis compared to those who get standard care.5 If you are worried that therapy might make things worse, you are not alone. The most up-to-date science shows that you do not need to stop drinking completely to benefit from trauma therapy, and starting this work is both safe and effective for people with ptsd and alcohol abuse.5, 8
Newer therapies—like mindfulness-based approaches and virtual programs—are also being studied for their ability to ease symptoms and fit into your life.10 Next, we will explore how these therapies are woven into treatment plans designed for dual recovery.
Treatment Approaches for PTSD and Alcohol Abuse
Therapy Models for Dual Recovery
When you are looking for help that truly addresses both ptsd and alcohol abuse, it is empowering to know there are specialized therapy models built just for your needs. Here is a simple assessment tool to guide you: Ask yourself—do you feel safer with a step-by-step approach, or do you want to address trauma memories and drinking patterns together from day one? Your comfort level can help you find the model that fits best.
One of the most researched options is Seeking Safety, which focuses on building coping skills before diving into painful trauma memories. This is a strong starting point if you want to feel more stable and learn tools to manage triggers. For those ready to work on both issues at once, approaches like COPE (Concurrent Treatment of PTSD and Substance Use Disorders Using Prolonged Exposure) blend trauma therapy and substance use counseling in the same sessions.
This strategy suits people who notice their trauma and alcohol use are closely connected and want to make progress on both, side by side. Studies confirm that integrated models like these are safe, effective, and can be adapted for group or individual therapy settings.5 You might also see programs that combine evidence-based therapies—such as Cognitive Processing Therapy or Trauma-Focused CBT—with regular check-ins about your substance use. These models work well for those who value structure and want to see steady progress in both areas.
Choosing a therapy model is a personal decision, and you deserve support that matches your pace and comfort level. Next, we will look at how medications can be paired with therapy to further support recovery from ptsd and alcohol abuse.
Medication-Assisted Treatment Options
Let’s start with a decision tool: Ask yourself—have you tried therapy for ptsd and alcohol abuse but still found cravings or anxiety hard to manage? If so, adding medication-assisted treatment (MAT) could be a supportive next step in your recovery.
Medication-assisted treatment brings together FDA-approved medications and counseling to address both trauma and alcohol use. For alcohol use, medicines like naltrexone and acamprosate help reduce cravings and prevent relapse, making it easier to focus on healing. For PTSD, selective serotonin reuptake inhibitors (SSRIs) such as sertraline and paroxetine are commonly prescribed to ease symptoms like anxiety, nightmares, or persistent sadness. You do not have to choose one or the other—these medications can be used alongside therapy for the best possible results.5
Regarding cost, generic versions of these medications are often covered by insurance with typical copays ranging from $10 to $50 per month, though prices vary based on your specific plan. If you are concerned about side effects or whether medications will change who you are, know that your healthcare team will work with you to find the safest, most effective options. Recent research is exploring promising new medications—like topiramate and cannabidiol (CBD)—that may help both ptsd and alcohol abuse at the same time.10
Opt for this approach when cravings, withdrawal, or severe mood swings make it tough to stay engaged in therapy alone, or if you want extra support during stressful times. Medication-assisted treatment is proven to be safe and effective, especially when paired with trauma-focused counseling.5 Next, we will discuss how to choose the right level of care and set yourself up for long-term recovery.
Building Your Path to Recovery
Choosing the Right Treatment Level
Choosing the right level of care is a critical decision. Use the interactive guide below to see which environment might best fit your current needs:
Inpatient or Residential Care
Best for: Individuals who need a safe place to step away from triggers and require 24/7 support.
Time Commitment: Typically 30 to 90 days living on-site.
Partial Hospitalization (PHP) or Intensive Outpatient (IOP)
Best for: People who can manage daily routines but need structured support while living at home.
Time Commitment: PHP is often 5 days a week (full days); IOP is usually 3-5 days a week for a few hours.
Flexible Outpatient & Virtual Programs
Best for: Those with full schedules, milder symptoms, or work/family commitments.
Time Commitment: 1-2 hours per week, often in evenings or via secure video calls.
Sober Living Homes
Best for: Individuals wanting a recovery-focused community bridge between treatment and independent life.
Time Commitment: Varies from a few months to a year or more.
Choosing the right level for ptsd and alcohol abuse often depends on symptom intensity, safety needs, and how much structure feels supportive. Research shows that matching care intensity to your needs improves outcomes and lowers relapse risk.5 Some people start with inpatient care, then step down to outpatient or virtual support as they gain stability.
This approach is ideal for those who want to build a strong foundation and gradually regain independence. Remember, treatment can be tailored—adjusting levels as your needs change. Every step you take, no matter how big or small, is a win on your path to recovery. Next, let’s look at common obstacles you might face and how to overcome them.
Overcoming Barriers to Getting Help
Let’s start with a quick self-assessment: Which of these barriers have you faced in seeking help for PTSD and alcohol abuse?
- Worry that treatment won’t work for you?
- Fear of being judged or misunderstood?
- Trouble finding care that addresses both trauma and alcohol use together?
- Not knowing where to start, or feeling overwhelmed by options?
- Concerns about balancing treatment with family, work, or daily life?
If any of these sound familiar, you are not alone. Many people feel stuck by these same challenges, but none of them mean recovery is out of reach. Research shows that integrated care—where trauma and alcohol use are treated together—works, even if you have not found success with past treatments or worry about setbacks.5
“You do not need to stop drinking before starting trauma therapy, and addressing both at once is proven safe and effective.”8
Systemic barriers, like separate mental health and addiction services, can make it harder to get the right support. If you are struggling to find a program that fits, consider reaching out to providers who offer integrated or virtual options, especially if you live in a rural area.10 Every step you take to overcome these barriers is a step toward healing. In the next section, we will answer common questions about recovery and what to expect along the way.
Frequently Asked Questions
Do I need to stop drinking completely before I can start trauma therapy for PTSD and alcohol abuse?
You do not need to stop drinking completely before starting trauma therapy for PTSD and alcohol abuse. Current research clearly shows that effective trauma-focused therapies are safe and beneficial even if you are still working on reducing your alcohol use 58. In fact, addressing both issues together—rather than waiting for full abstinence—can actually support better outcomes for many people. Your healing journey can begin right where you are, and you deserve care that meets you with compassion and flexibility. You are not alone in this process, and taking the first step toward help is already a big achievement.
How long does integrated treatment for PTSD and alcohol abuse typically take to show results?
You might wonder when you’ll start to feel better with integrated treatment for PTSD and alcohol abuse. Most people begin noticing improvements within the first few weeks, especially as therapy and support start to address both trauma and drinking patterns together. Research shows that it can take about three to four months for meaningful changes, but everyone’s pace is different—and that’s okay 5. Some people see steady progress early on, while others may need longer to feel lasting relief. The important thing is to keep moving forward and give yourself credit for every positive step. Recovery is a journey, not a race.
Can virtual treatment programs effectively address both PTSD and alcohol abuse if I live in a rural area?
Yes, virtual treatment programs can effectively address both PTSD and alcohol abuse, even if you live in a rural area. Recent studies confirm that online therapy options—like virtual Intensive Outpatient Programs (IOP)—deliver evidence-based care for both trauma and substance use, helping you overcome barriers related to distance or limited local resources 10. You’ll get access to proven therapies such as Cognitive Processing Therapy and Trauma-Focused CBT through secure video sessions, group support, and digital resources. This approach works well if travel or finding in-person specialists is tough, and it lets you connect with care from home. You deserve support, wherever you are.
Will addressing my trauma make my alcohol use worse during treatment?
It’s common to worry that talking about trauma might make alcohol use worse during treatment for PTSD and alcohol abuse. However, studies have shown that addressing trauma in therapy does not increase drinking or cause setbacks—instead, it often leads to real progress in both areas 58. When you work on the root causes of distress, you’re actually giving yourself a stronger foundation for change. In fact, improvements in trauma symptoms are linked to lower substance use over time 10. You deserve care that meets you where you are, and integrated treatment is proven to be both safe and effective.
How do I choose between different therapy approaches like Prolonged Exposure and Cognitive Processing Therapy for PTSD and alcohol abuse?
Choosing between Prolonged Exposure (PE) and Cognitive Processing Therapy (CPT) for PTSD and alcohol abuse depends on what feels most comfortable and helpful for you. PE is a good fit if you want to gradually face traumatic memories in a safe, structured way, helping to reduce fear and avoidance. CPT might work better if you prefer to focus on changing unhelpful beliefs and thoughts about your trauma, especially if guilt or self-blame are major challenges. There isn’t a single “best” option—both are proven therapies, and research shows that either can be effective for people with ptsd and alcohol abuse 56. Trust your instincts and talk with your provider about what approach matches your needs.
What ongoing support will I need after completing initial treatment for PTSD and alcohol abuse?
After finishing initial treatment for PTSD and alcohol abuse, ongoing support is so important for long-term healing. This can include regular check-ins with a therapist, joining mutual-help groups like SMART Recovery or AA, participating in alumni programs, or attending family therapy sessions. Research shows that continuing care—meaning structured, ongoing support after primary treatment—leads to better recovery outcomes and lowers the risk of relapse 7. You might also benefit from peer mentorship or periodic virtual sessions to stay connected. Building a strong support system helps you handle stress and celebrate your progress as you keep moving forward.
Can I maintain my job and family responsibilities while getting help for PTSD and alcohol abuse?
You absolutely can maintain your job and family responsibilities while getting help for PTSD and alcohol abuse. Many treatment programs are designed with flexibility in mind, such as evening or virtual Intensive Outpatient Programs (IOP), which let you fit therapy sessions around work and home life. Research supports that integrated care can be tailored to your schedule, making it possible to balance recovery with daily commitments 5. If you’re worried about taking time off, know that even small steps—like weekly counseling or online support—make a difference. Your dedication to both healing and your loved ones is a strength, not a barrier. You deserve support that fits your real life.
Your Next Steps Toward Healing
Taking the first step toward recovery can feel overwhelming, but you do not have to navigate this journey alone. Start by reaching out to a healthcare professional who specializes in substance use disorders. They can provide an honest assessment of your situation and recommend appropriate treatment options tailored to your needs.
Consider connecting with a treatment center that offers comprehensive care, including medical detox, therapy, and ongoing support. Many facilities provide free consultations to help you understand what recovery might look like for you. Do not hesitate to ask questions about their approach, success rates, and the types of therapies they offer.
If you are not ready for formal treatment, begin by building a support network. Reach out to trusted friends or family members who can encourage you along the way. Attend local support group meetings where you will meet others who understand what you are experiencing.
Remember, seeking help is a sign of strength, not weakness. Every person’s recovery journey is unique, and what matters most is that you are taking action today. Your path to healing starts with one decision—the decision to ask for help.
References
- Comorbidity of posttraumatic stress disorder and substance use disorders. https://pubmed.ncbi.nlm.nih.gov/22791374/
- Posttraumatic stress disorder and substance use disorders: A review of the research. https://psycnet.apa.org/record/2012-16327-002
- Concurrent treatment of substance use and PTSD. https://pubmed.ncbi.nlm.nih.gov/24928573/
- Alcohol use disorder (AUD) in the United States: Age groups and demographic characteristics. https://www.niaaa.nih.gov/alcohols-effects-health/alcohol-topics/alcohol-facts-and-statistics/alcohol-use-disorder-aud-united-states-age-groups-and-demographic-characteristics
- Treatment of comorbid posttraumatic stress disorder and substance use disorders. https://www.ptsd.va.gov/professional/articles/article-pdf/id1635224.pdf
- Treating PTSD: A review of evidence-based psychotherapy interventions. https://pubmed.ncbi.nlm.nih.gov/18074252/
- Impact of continuing care on substance use disorder recovery. https://pubmed.ncbi.nlm.nih.gov/24695242/
- A systematic review of trauma interventions in Native communities. https://pmc.ncbi.nlm.nih.gov/articles/PMC7243818/
- Clinical practice guideline for the treatment of posttraumatic stress disorder. https://www.apa.org/ptsd-guideline
- Alcohol use disorder & traumatic stress research. https://med.nyu.edu/departments-institutes/psychiatry/research/alcohol-use-disorder-traumatic-stress





