Key Takeaways: Your Path to Integrated Recovery
- Integrated Care is Essential: Treating mental health and substance use simultaneously via outpatient dual diagnosis reduces hospitalization risks and improves long-term outcomes.
- Flexible Options Exist: Choose between Partial Hospitalization (PHP) for daily structure or Intensive Outpatient (IOP) to balance work and recovery.
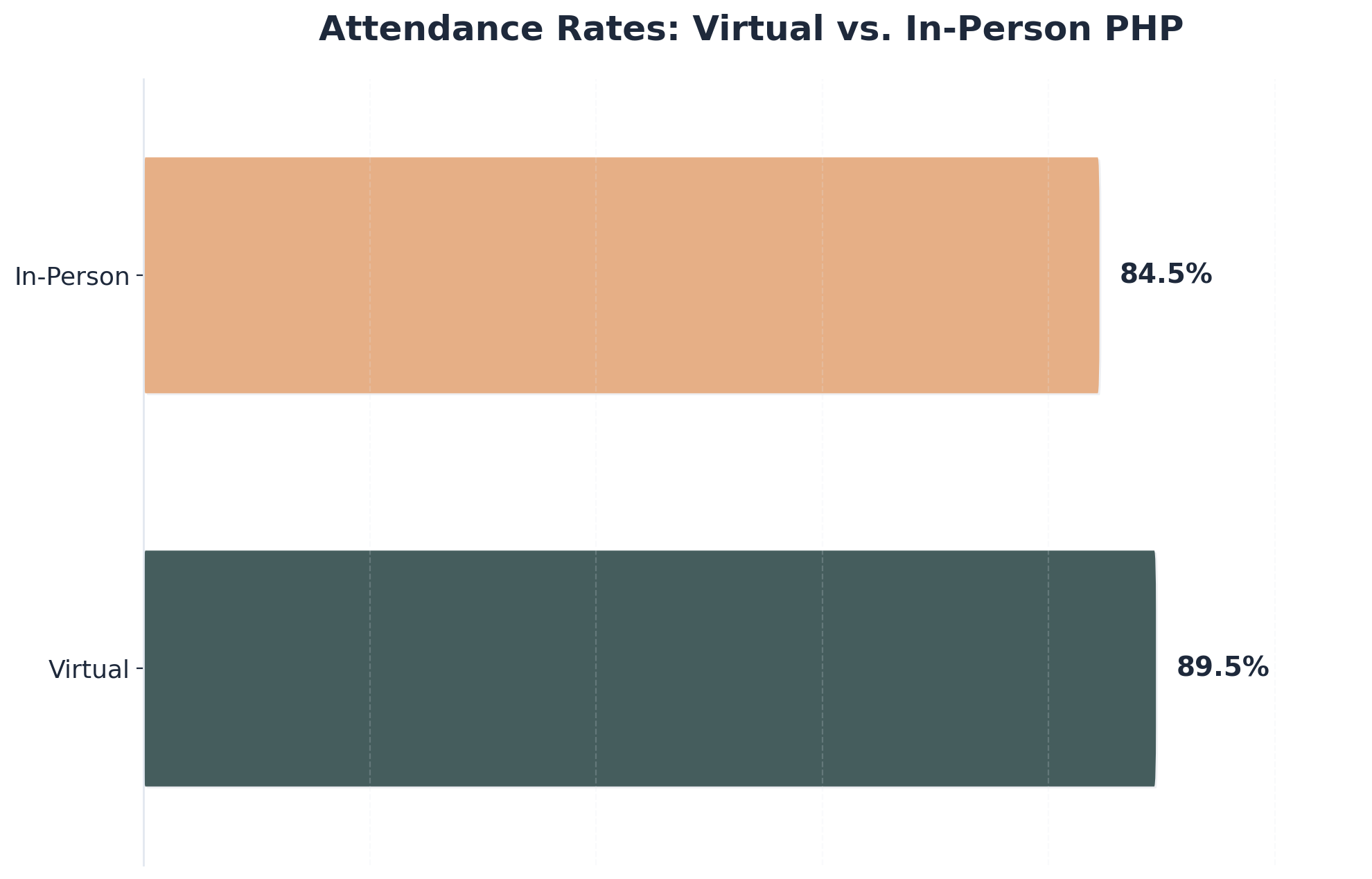
- Virtual Access Works: Telehealth programs show high attendance rates (89.5%) and are effective for those with transportation or rural barriers.
- Insurance Support: Most major carriers cover integrated care; verifying your benefits is the first actionable step.
- Timeline for Healing: Expect an 8–12 week initial commitment, with the first 30 days focused on stabilization and skill-building.
Understanding Your Outpatient Dual Diagnosis Journey
When you are navigating the complexities of a psychiatric condition alongside addiction, finding the right path forward is critical. This combination, known as co-occurring disorders, requires a specialized approach called outpatient dual diagnosis treatment. Unlike traditional methods that treat issues separately, this integrated model addresses both conditions simultaneously, recognizing that your mental health and substance use are deeply interconnected.
- Do your anxiety or depression symptoms seem to trigger substance use?
- Does using substances make your mental health symptoms feel more intense later?
- Have you tried treating one issue (like addiction) only to have the other (like depression) cause a setback?
Comprehensive integrated care operates on the understanding that psychiatric conditions and addiction often fuel each other in a cyclical pattern. For example, untreated anxiety may lead to alcohol use as a coping mechanism, which in turn destabilizes your mood further. Outpatient dual diagnosis programs break this cycle by coordinating therapies for both issues under one roof.
“Research shows that integrating care for both conditions in a single program leads to fewer hospitalizations, less substance use, and better overall results compared to treating each issue on its own.”1, 3
Why Previous Treatments May Have Failed
If you have attempted recovery before without success, it is likely not a failure of will, but a failure of the treatment model. Many standard programs focus exclusively on either mental health or substance use. This “siloed” approach leaves half of your struggle unaddressed. Studies indicate that individuals with co-occurring conditions are 1.7 times more likely to experience relapse or emergency visits when only one issue is treated.3
Outpatient dual diagnosis care reduces these risks by:
- Reducing Hospitalizations: Integrated outpatient programs are associated with fewer psychiatric hospitalizations compared to single-focus programs.1
- Improving Engagement: Virtual outpatient options have shown hospitalization rates dropping to as low as 8.9%, compared to 16.5% for traditional in-person care, largely due to increased accessibility.4
- Skill Retention: You learn coping mechanisms that apply to both stress management and craving reduction simultaneously.
Decision Framework: Choosing Outpatient Dual Diagnosis Care
Deciding between residential care and outpatient dual diagnosis treatment is a pivotal moment in your recovery. This decision should be based on clinical necessity, daily responsibilities, and your current support system. Use the comparison below to help guide your choice.
| Feature | Residential / Inpatient | Partial Hospitalization (PHP) | Intensive Outpatient (IOP) |
|---|---|---|---|
| Time Commitment | 24/7 Supervision (30-90 days) | 5 days/week (6-8 hours/day) | 3-5 days/week (3 hours/session) |
| Living Situation | Live at the facility | Live at home | Live at home |
| Best For | Severe instability, safety risks, or lack of home support. | High medical/clinical need but safe to return home at night. | Moderate stability; need to balance work/family. |
| Work/School | Medical leave usually required. | Medical leave often required. | Can often continue working/school. |
Evaluating PHP vs. IOP Structures
Within the realm of outpatient dual diagnosis, you will typically choose between Partial Hospitalization Programs (PHP) and Intensive Outpatient Programs (IOP).
Partial Hospitalization (PHP): This is the highest level of outpatient care. It acts as a bridge between inpatient and outpatient, providing daily medical monitoring and intensive therapy. It is ideal if you need significant structure but have a safe home environment.
Intensive Outpatient (IOP): This level offers greater flexibility. Sessions often run in the evenings or weekends, allowing you to maintain employment. Research confirms that both PHP and IOP models effectively reduce relapse and hospitalizations when they utilize integrated care models.1, 3
Overcoming Barriers: Virtual and Flexible Options
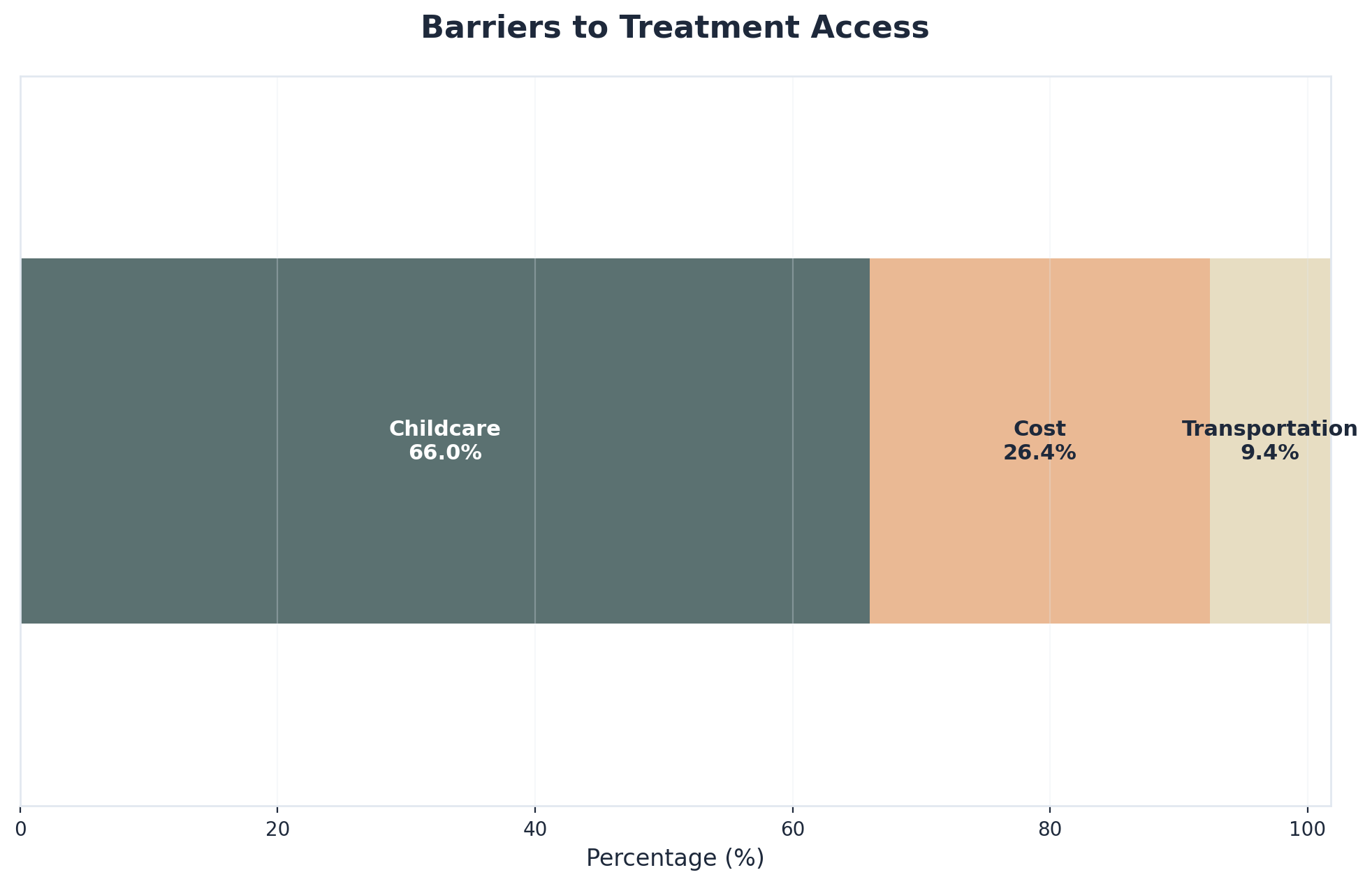
Barriers such as geography, work schedules, and childcare often prevent access to care. However, modern outpatient dual diagnosis programs have evolved to meet these challenges.
Living in a Rural Area?
Virtual outpatient programs are now a robust alternative. Studies show virtual attendance rates can reach 89.5% (higher than in-person), with excellent clinical outcomes. This brings evidence-based therapy and medication management directly to your home via secure video calls.4
Balancing a Career?
Flexible scheduling, including evening tracks, allows professionals to engage in outpatient dual diagnosis treatment without sacrificing their livelihood. High engagement rates in these flexible programs suggest that maintaining employment can actually serve as a stabilizing factor during recovery.4
Resource Planning and Treatment Components
Entering treatment requires practical preparation. Understanding the financial and logistical requirements of outpatient dual diagnosis care helps remove uncertainty and allows you to focus entirely on healing.
Financial and Insurance Navigation
Cost is a primary concern for many, but coverage for integrated care has expanded significantly due to parity laws. Most major insurance carriers now include outpatient dual diagnosis services as standard benefits.
Actionable Steps for Insurance Verification:
- Call the member services number on the back of your insurance card.
- Ask specifically: “Does my plan cover integrated behavioral health services or co-occurring disorder treatment?”
- Request details on copays for IOP or PHP levels of care.
- Ask if prior authorization is required from your primary care physician.
If you face gaps in coverage, ask treatment centers about sliding scale fees or payment plans. Investing in integrated care is cost-effective in the long run, as it is linked to lower total healthcare costs compared to treating conditions separately.1, 6
Core Clinical Components
Effective outpatient dual diagnosis programs rely on evidence-based therapies. You should expect your treatment plan to include:
- CBT & DBT: Cognitive Behavioral Therapy helps identify triggers, while Dialectical Behavior Therapy focuses on emotional regulation and distress tolerance. These are proven to reduce relapse risk.1
- Medication-Assisted Treatment (MAT): Using FDA-approved medications alongside therapy can stabilize brain chemistry. Research indicates that combining medication with therapy leads to better retention and fewer positive drug screens than therapy alone.5
- Peer Support: Group sessions provide a community of understanding, reducing the isolation often felt in early recovery.
Your Next 30 Days: Building a Foundation
The first month of outpatient dual diagnosis treatment is about stabilization and routine. Knowing what to expect week-by-week can help manage anxiety.

- Week 1: Assessment & Stabilization
Your journey begins with a comprehensive evaluation, often using ASAM Criteria to determine your specific needs.10 You will meet your care team, start medication management if needed, and begin attending group sessions. The focus is on physical safety and immediate symptom management. - Weeks 2-3: Skill Acquisition
You will dive deeper into therapies like CBT and DBT. You will establish a daily routine—waking up at a set time, attending sessions, and practicing mindfulness. This structure is crucial for resetting your body’s natural rhythms. - Week 4: Integration & Planning
By the end of the first month, you will start applying coping skills to real-world triggers. You will also begin discussing “step-down” planning or continuing care options to ensure you have long-term support after the intensive phase ends.
The Importance of Continuing Care
Recovery does not end after 30 days. Structured continuing care—such as regular check-ins, alumni groups, or living in recovery housing—is strongly recommended. Research shows that maintaining connection with a support network significantly improves abstinence rates and helps individuals return to treatment faster if a slip occurs.7, 8
Frequently Asked Questions
As you explore comprehensive co-occurring disorder support, you likely have questions about what to expect. Here are answers to common concerns regarding outpatient dual diagnosis care.
What makes outpatient dual diagnosis treatment different from treating my mental health and substance use separately?
Outpatient dual diagnosis treatment stands apart because it addresses your mental health and substance use challenges together, not in isolation. When these issues are treated separately, important connections between your symptoms and behaviors can be missed. Research shows that integrating care for both conditions in a single program leads to fewer hospitalizations, less substance use, and better overall results compared to treating each issue on its own.1, 3
How do I know if I need outpatient dual diagnosis treatment instead of residential care?
You might benefit from outpatient dual diagnosis treatment if you feel safe at home, can manage daily routines, and want to stay connected to work, family, or school while getting care. Residential care is better if you’re facing severe symptoms, safety risks, or need a highly structured environment for stability. Research shows integrated outpatient options reduce hospitalizations and support long-term wellness.1, 3
Can I continue working while attending outpatient dual diagnosis treatment?
Yes, you can continue working. These programs are designed for people who want to maintain their jobs, education, or family responsibilities. Many outpatient dual diagnosis programs offer flexible scheduling, including evening or weekend sessions. Studies show that flexible and virtual outpatient programs reach nearly 90% attendance rates.4
What if I live in a rural area with no local outpatient dual diagnosis treatment programs?
Virtual outpatient dual diagnosis services are widely available. Research shows these virtual programs actually achieve higher attendance (89.5%) and lower psychiatric hospitalization rates (8.9%) compared to in-person care, allowing you to access evidence-based therapy and medication management from home.4
Will my insurance cover outpatient dual diagnosis treatment?
Many insurance plans cover outpatient dual diagnosis treatment due to parity laws requiring mental health coverage to match medical coverage.6 Most major carriers include integrated behavioral health services. It is best to call your insurance company to verify specific benefits and network providers.
What is the difference between PHP and IOP in outpatient dual diagnosis treatment?
PHP (Partial Hospitalization) is more intensive, typically involving therapy 5 days a week for several hours, while IOP (Intensive Outpatient) offers more flexibility, usually meeting 3-5 times a week. Both settings use integrated behavioral health services to address co-occurring disorders.1, 3
How long does outpatient dual diagnosis treatment typically last?
A typical stay might last 8–12 weeks, but the duration depends on your needs. Some find that ongoing support through step-down care helps sustain recovery beyond the initial phase.7 Your care team will adjust the duration to match your goals.
Can outpatient dual diagnosis treatment include medication management?
Yes, medication management is often included. Licensed providers can prescribe FDA-approved medications to manage cravings or stabilize mood. Research shows that combining medication with talk therapy leads to better engagement and lower rates of substance use compared to therapy alone.5
Is continuing care necessary after completing outpatient dual diagnosis treatment?
Yes, continuing care is strongly recommended. Research shows that structured continuing care—such as regular check-ins or support groups—leads to better substance use outcomes and helps people return to treatment faster if setbacks happen.7
Start Your Integrated Recovery Journey Today
Taking the first step toward healing from co-occurring psychiatric and addiction disorders requires courage, and you don’t have to walk this path alone. A comprehensive integrated treatment approach addresses all aspects of your wellbeing simultaneously, giving you the best opportunity for lasting recovery.
The journey begins with reaching out. Whether you’re struggling with depression and alcohol use disorder, anxiety and chemical dependence, or any combination of psychiatric and addiction challenges, specialized outpatient dual diagnosis programs can provide the coordinated care you need. These programs recognize that your psychological condition and addiction are interconnected, requiring simultaneous attention from a multidisciplinary team.
Many people wait for the “perfect moment” to seek help, but that moment is now. Call today for a free, confidential assessment where you can discuss your specific situation without pressure or judgment. Speak with an admissions counselor who can verify your insurance coverage, answer your questions about integrated treatment, and help you understand exactly what coordinated care looks like. You deserve comprehensive care that treats the whole person—mind, body, and spirit.
References
- Health outcomes and service use patterns associated with co-located mental health and AOD specialist treatment. https://pmc.ncbi.nlm.nih.gov/articles/PMC10946517/
- Effectiveness of Integrated Dual Diagnosis Treatment (IDDT) in severe mental illness outpatients with a co-occurring substance use disorder. https://pubmed.ncbi.nlm.nih.gov/30352668/
- Concurrent Disorders and Treatment Outcomes: A Meta-Analysis. https://www.tandfonline.com/doi/full/10.1080/15504263.2025.2515015?src=exp-la
- Positive Outcomes in a Virtual Partial Hospitalization Program. https://pmc.ncbi.nlm.nih.gov/articles/PMC9395212/
- The Impact of Addiction Medications on Treatment Outcomes for Individuals with PTSD. https://pmc.ncbi.nlm.nih.gov/articles/PMC4866634/
- Treatment Access Barriers and Disparities Among Individuals with Co-Occurring Substance Use and Mental Health Disorders. https://pmc.ncbi.nlm.nih.gov/articles/PMC4695242/
- Impact of Continuing Care on Recovery From Substance Use Disorder. https://pmc.ncbi.nlm.nih.gov/articles/PMC7813220/
- The Role of Recovery Housing During Outpatient Substance Use Treatment. https://pmc.ncbi.nlm.nih.gov/articles/PMC8748296/
- Common Comorbidities with Substance Use Disorders Research. https://www.ncbi.nlm.nih.gov/books/NBK571451/
- About The ASAM Criteria. https://www.asam.org/asam-criteria/about-the-asam-criteria





